HIGHLIGHTS
- What is already known about this subject:
Endoscopy is routinely performed for the evaluation of H. pylori-associated diseases.
White light endoscopy (WLE) impression alone is often inaccurate and has poor sensitivity to identify H. pylori. - What are the new findings:
Narrow band imaging (NBI) exhibits better sensitivity compared to WLE in identifying H. pylori-associated gastritis.
Patients with higher grades of NBI (≥3) were 14.2 times more likely to have H. pylori-positive gastritis on histopathology.
ABSTRACT – Background
Conventional white light endoscopic (WLE) findings of H. pylori-associated gastritis are often non-specific and may not correlate with histology. Narrow band imaging (NBI), an optical digital technique employed for the visualization of vessels and patterns of gastric mucosa may improve identification. We evaluated the role of NBI in detecting H. pylori-associated gastritis and classifying its severity.
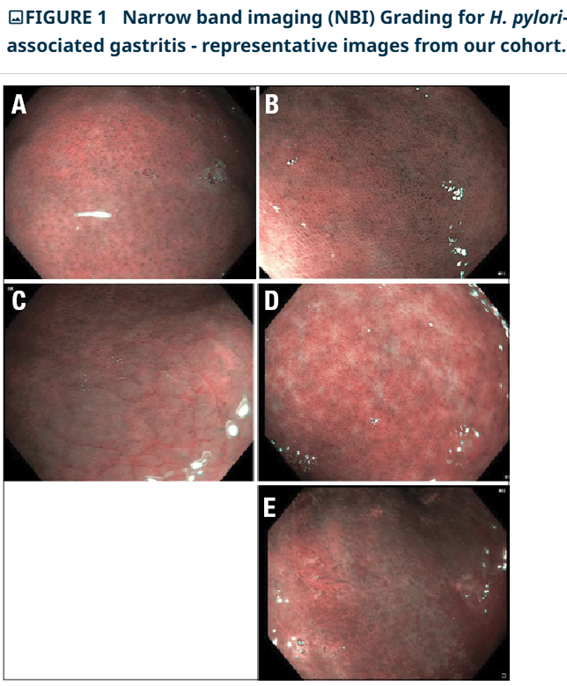
Methods: Institution-based prospective observational study conducted between May 2021-October 2022. Children presenting with chronic abdominal pain (>1-month duration) were evaluated. Eligible children underwent gastroscopy with NBI and gastric biopsies for rapid urease test and histopathology. NBI gastroscopic findings were classified into five grades as per the classification by Alboudy et al. The association of NBI grade with the presence and severity of H. pylori gastritis on histopathology was analysed.
Results: Ninety children (mean age 12.65±3.91 years), 52 (57.7%) males with median duration of symptoms of 4.5 (3-12) months underwent gastroscopy. H. pylori was detected on histopathology in 29 (32%) patients. NBI findings suggested a mucosal abnormality in 27/29 (93.1%) children with H. pylori on histopathology. H. pylori positive gastritis was significantly more common among those with higher (≥3) NBI grades as compared to those with lower NBI grades (61% vs10%, P<0.001). No significant association was found between NBI grade and the severity of H. pylori gastritis (P=0.75). NBI exhibited better sensitivity (0.82) compared to WLE (0.55) in identifying H. pylori-associated gastritis. On receiver operating characteristic curve analysis, NBI had higher area under curve (0.79 vs 0.65) as compared to WLE.
Conclusion: NBI morphological pattern is a useful tool in identifying patients with H. pylori-associated gastritis.
AUTORES
SEMWAL, Pooja BOLIA, Rishi BHAT, Nowneet Kumar PATNAIK, Itish DURGAPAL, Prashant SHARMA, Rahul