HIGHLIGHTS
- Hepatopulmonary syndrome (HPS) is not an uncommon complication of cirrhosis in children and adolescents, particularly when biliary atresia is the underlying condition.
- Screening with pulse oximetry (O2 saturation <96%), unlike in adults, has low sensitivity in the pediatric age group.
- No differences were found in post-liver transplantation mortality between children of different hypoxemia ranges, contrary to findings from adults.
- There are still many gaps to be filled regarding the condition and not all data obtained in studies with adults reflects the disease’s behavior in pediatrics, especially concerning prognosis.
ABSTRACT – Background –
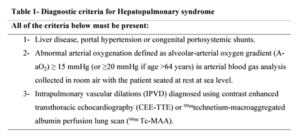
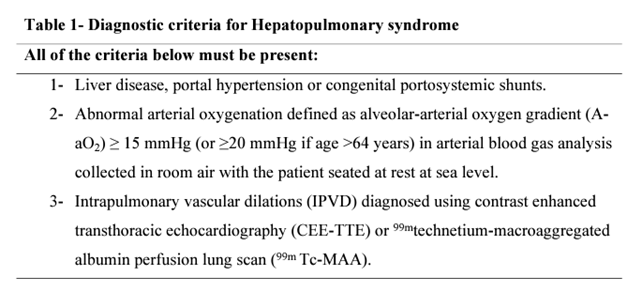
Hepatopulmonary syndrome (HPS) is characterized by the triad of abnormal arterial oxygenation caused by intrapulmonary vascular dilatations (IPVD) in the setting of advanced liver disease or portal hypertension, impacting the patient’s quality of life and survival. There are still many gaps in the literature on this topic, especially in pediatrics, with practices frequently based on extrapolation of data obtained from adults. Objective – Provide a synthesis of the current knowledge about HPS in children. Methods – The research was carried out through narrative review. The databases used for the search include Medline, Embase, Elsevier, Lilacs and Scielo. The key words used were “hepatopulmonary syndrome” AND child, children, infant, preschool, pediatric. Results – In cirrhotic children, the prevalence of HPS can reach up to 42.5%, and it is even more common in those whose underlying condition is biliary atresia, reaching up to 63%. Screening with pulse oximetry (O2 saturation <96%), unlike in adults, has low sensitivity in the pediatric age group. Management involves supportive care with oxygen therapy; liver transplantation is the only definitive treatment to reverse the condition, and HPS is considered an exceptional criterion for the waitlist. The waitlist mortality is similar among children listed by HPS as a special criterion when compared to those listed for other reasons. The reported rates of complete resolution of hypoxemia after liver transplantation are close to 100% in children. The post-liver transplantation survival is similar or slightly lower in children with HPS when compared to those without HPS. Contrary to findings from adults, no differences were found in post-liver transplantation mortality between children of different hypoxemia ranges, although longer mechanical ventilation time and hospital stay were observed in children with PaO2 <50 mmHg. Conclusion – HPS is not an uncommon complication of cirrhosis in children and adolescents, particularly when biliary atresia is the underlying condition. There are still many gaps to be filled regarding the condition, and this article demonstrates that not all data obtained in studies with adults reflects the disease’s behavior in pediatrics, especially concerning prognosis.
AUTORES
Letícia Drumond ALBERTO¹, Eleonora Druve Tavares FAGUNDES1,2, Adriana Teixeira RODRIGUES1,2, Thaís Costa Nascentes QUEIROZ¹, Gustavo Valverde de CASTRO2 and Alexandre Rodrigues FERREIRA1,2